By David Malmo-Levine and Rob Callaway, M.A., 2012
Table of Contents
Cannabis, Cure-Alls, and Evidence…………………………………………… 3
The Endocannabinoid System…………………………………………………… 3
Stress and Anxiety…………………………………………………………………… 4
Anxiolytics, Hypnotics, Narcotics, Nervines, Relaxants, Sedatives, and Soporifics…………………………………………………………………………. 5
The History of the Use of Cannabis as an Anxiolytic, Hypnotic, Narcotic, Nervine, Relaxant, Sedative, and Soporific………………….. 6
The Ancient Era…………………………………………………………………… 6
The Scientific Era………………………………………………………………… 9
Medical Indexes and Textbooks: Lying About the Risks but Telling the Truth About the High………………………………………. 11
Government Reports……………………………………………………….. 12
Cross-Cultural Use………………………………………………………….. 13
Recent Studies………………………………………………………………… 14
Comparisons With Synthetic Medicines…………………………….. 20
Cannabis as Preventive Medicine……………………………………… 22
Beginning to Understand the Nuances of Cannabis Medicine.. 24
What About the Smoke?……………………………………………………… 26
Conclusion…………………………………………………………………………. 26
References……………………………………………………………………………. 28
Cannabis, Cure-Alls, and Evidence
History teaches us that we should all be wary of cure-all claims. Therefore, it is understandable that many physicians are reluctant to accept what appear, at face-value, to be exaggerated claims made by cannabis consumers in relation to the therapeutic benefits derived from their use of the plant. This one plant and its numerous active compounds, it is claimed, seem to positively affect nearly every ailment of our minds and bodies, from mental illness to cancer. Is this possible?
In short, yes. In fact, there is no shortage of evidence to substantiate many of these claims. The last couple of decades have seen an incredible explosion of research exploring the potential therapeutic applications of cannabis and cannabis-derived medications. Today, more evidence is available in relation to the positive therapeutic applications of cannabis than is available for some of the most widely used conventional medications and therapies (Sulak, 2011).
The Endocannabinoid System
It is widely understood, although not as widely recognized by the medical community, that cannabis is both powerful and safe, and can alleviate the suffering of dozens of severe chronic and acute medical conditions. How is it possible that one plant can do so much? The answer lies in the fairly recently discovered physiologic system known as the endocannabinoid system, which plays a role in modulating and regulating nearly every bodily function in all vertebrates (de Fonseca et al., 2005; Gieringer, Rosenthal, & Carter, 2008; Grotenhermen, 2006a). Our bodies naturally produce five known chemical compounds called endogenous cannabinoids, or endocannabinoids (de Fonseca et al.; Grotenhermen, 2006b), similar in structure and action to the chemical compounds found most abundantly in cannabis, called phytocannabinoids, of which at least 85 have been identified and isolated from the plant (El-Alfy et al., 2010).
These naturally occurring compounds and their two known receptors, CB1 and CB2, are found virtually everywhere in the human body, from the brain, organs, connective tissues and glands, to immune cells (Grotenhermen, 2006a, 2006b; Sulak, 2011). Despite different functions of the endocannabinoid system, which depend upon the location in the body of the receptors of interest, the goal is constant: homeostasis, or “the maintenance of a stable internal environment despite fluctuations in the external environment” (Sulak, 2011, p. 11; Melamede, 2005). In fact, cannabinoids promote homeostasis at every level of biological life, from the sub-cellular to the whole organism, and thus, the endocannabinoid system is a global homeostatic regulator (Melamede, 2005). It is estimated that the endocannabinoid system evolved over 600 million years ago, and is now shared by all vertebrates as an essential part of adaptation to environmental changes, and thus, an essential part of life (Guzmán, 2005; Melamede, 2005; Sulak, 2011). Therefore, the endocannabinoid system is a central component of both health and healing, perhaps the most important system (Melamede, 2005; Sulak, 2011).
Stress and Anxiety
Dr. Hans Selye discovered a damaging syndrome in rats in response to nonspecific nocuous agents (Selye, 1936/1998), now known as the “stress concept” (Selye, 1976, p. 53). He coined and defined the term stress, in relation to physiology, as “…the nonspecific response of the body to any demand” (Selye, 1973, p. 692, Selye, 1976, p. 53). However, Selye emphasized that stress has two components, distress, which is bad stress, and eustress, which is good stress (Selye, 1976). Our bodies respond nearly identically to both forms of stress; however, eustress causes far less damage to us than does distress, largely due to our ability to more readily adapt to eustress than to distress, but which form stress takes is largely subjective; what is eustress to one person may be distress to another (Selye, 1976).
The definition of stress has been adapted and modified over time. For instance, Hoerr and Osol (1952, p. 697) define stress as “a loading of the nervous system”, while The Bantam Medical Dictionary of 1990 defines it as “any factor that threatens the health of the body or has an adverse effect on its functioning, such as…worry” (“Stress”, 1990, pp. 414-415). A stress reaction has been defined as “a response to extreme anxiety” and “…treatment for a stress reaction includes the use of drugs to calm the patient…” (Glanze, Anderson, & Anderson, 1987a, p. 547). Although there is no consensus definition of stress, since Selye’s initial writings chronic stress (more appropriately, chronic distress) has become widely recognized as a leading cause of death in the industrialized world due to its major contribution to killers such as heart disease, the development and relapse rates of major depression (which is also a major independent contributor to heart disease), and the progression of HIV to AIDS (Cohen, Janicki-Deverts, & Miller, 2007). Thus, any intervention that may effectively decrease chronic stress, while not being a further burden to ill health, is an important ally and should be pursued.
Anxiety is defined as “a feeling of worry, upset, uncertainty, and fear that comes from thinking about some threat or danger” (Glanze et al., 1987b, p. 39). For anxiety attack and anxiety neurosis, Glanze et al. indicate “treatment may include drugs and psychotherapy” (p. 39). More contemporarily, the American Psychological Association (APA) (APA, n.d.) defines anxiety as “an emotion characterized by feelings of tension, worried thoughts and physical changes like increased blood pressure”. Importantly, anxiety is becoming increasingly recognized as an independent factor contributing to coronary heart disease and mortality (e.g., Roest, Martens, de Jonge, & Denollet, 2010; Shen et al., 2008), and therefore, interventions that reduce anxiety are allies and should be implemented.

Anxiolytics, Hypnotics, Narcotics, Nervines, Relaxants, Sedatives, and Soporifics
Taber’s Cyclopedic Medical Dictionary defines an anxiolytic as “a drug that relieves anxiety” (Venes et al., 2001a, p. 138). Dorland (1903a), in The American Illustrated Medical Dictionary, defines soporific as an agent “causing or producing profound sleep” (p. 635), hypnotic as “a drug that produces sleep” (1903b, p. 327), a relaxant as “an agent that lessens tension” (1903c, p. 587), a nervine as “allaying nervous excitement…a remedy for nervous disorders” (1903d, p. 457), and a sedative as “a remedy that allays excitement” (1903e, p. 615). Dorland (1903f, p. 615) further defines a cerebral sedative as “one which particularly affects the brain. To this class belong cannabis [emphasis added], camphor, the bromids, hyoscin, and the hypnotic and revulsive agents”. Dorland (1903e, p. 615) also includes cannabis in a list of the nerve-trunk sedatives.
Narcotic was originally just another name for a drug that produced “sleep or stupor” (Dorland, 1903g, p. 445, Dorland, 1960, p. N-1), and therefore, some early sources list cannabis as one of the primary narcotics (e.g., Hoerr & Osol, 1952). But in many parts of the medical world the term narcotic has come to be associated exclusively with drugs “more powerful than hypnotics” (Taber et al., 1952, p. N-3), such as opiates and other drugs that produce physical withdrawal symptoms (Glanze et al., 1987c, p. 395). Because cannabis’ withdrawal symptoms have historically been described as mild (e.g., “Marihuana”, 1950, p. 1102; Schifferes, 1963, p. 349), and further confirmed to be so by recent government reviews of all available evidence (e.g., Nolin, Kenny, Banks, Maheu, & Rossiter, 2002, pp. 137, 152, 154, 163, 193), narcotic as applied to cannabis is no longer appropriate, and is now an opiate-specific term (“Narcotic”, 1990).
Importantly, the current government-sanctioned medical definitions of the terms above have changed little over time
(e.g., www.nlm.nih.gov/medlineplus/mplusdictionary.html).
The History of the Use of Cannabis as an Anxiolytic, Hypnotic, Narcotic, Nervine, Relaxant, Sedative, and Soporific
Within the long history of medical literature concerning cannabis there are many differing views about the risks associated with the use of cannabis, as well as varying opinions about the causes of those risks. However, as to the effects of cannabis, its reputation as an anxiolytic, hypnotic, narcotic, nervine, relaxant, sedative, and soporific has remained a constant through thousands of years of documented use, including up to the present day.
The Ancient Era
Some of the first recorded benefits of cannabis use were to treat stress and anxiety. The earliest known description of cannabis or hashish (note: hashish or hasheesh is a concentrated extract of whole cannabis) as a treatment for stress and anxiety appear in ancient Sumerian texts, where cannabis was called the “plant of forgetting worries” (as cited in Rätsch, 1998/2001, p. 82). Russo (2007) further points to the work of Thompson, who spent 50 years deciphering medical texts from the Bronze Age civilization of Assyria, whose translation of a cuneiform word argued to be for cannabis, GAN.ZI.GUN.NU (c. 2000 B.C.E), equates to “the weaving narcotic” (p. 1629). In addition, in a 2003 personal communication from the British Museum, Russo (2007, p. 1630) reports that an Assyrian clay tablet listing synonyms for cannabis includes a word translated as ‘for or against panic’.
Furthermore, in the Atharvaveda (c. 1400 B.C.E.) cannabis (the bhang plant) is mentioned once: “We tell of the five kingdoms of herbs headed by Soma; may it and kuca grass, and bhanga and barley, and the herb saha release us from anxiety” (passage 11.5.16, as cited in Grierson, 1894, p. 246). The Zend-Avesta, a Persian equivalent of the Vedas, and allegedly written by Zarathustra – also known as Zoroaster – in the 7th century B.C.E. refers to concoctions made from cannabis as Zoroaster’s “good narcotic” (Müller, 1883, p. 267).
In the famous Book of a Thousand Nights and a Night, better known as Arabian Nights, a collection of tales dating from the Islamic Golden Age (c. 750 C.E. – c. 1258 C.E.), bhang is mentioned many times in relation to producing sleep. For instance there is the story of King Omar causing Princess Abrizah to fall into a deep sleep by using a piece of concentrated “Bhang” (Burton, 1706/2003, pp. 122-123). Several hundred years later, in 1563, Garcia Da Orta (1563/1895, p. 55), physician, pioneer of tropical medicine, and naturalist, wrote that bangue, an Indian drink made with cannabis, could raise a man “…above all cares and anxieties…”, and at approximately the same time, in China, Li Shih-Chen (or Li Shizhen) included cannabis sativa in his famous and comprehensive 1578 (first published 1593) herbal Pen-ts’ao kang mu as a remedy for “nervous disorders” (Li Shih-Chen, 1593/1911, p. 91). Furthermore, in the Rajvallabha, a 17th century Materia Medica dealing with drugs used in India, ganja (cannabis) is said to be a “… desire-fulfilling drug [that] was obtained by men on earth, through desire for the welfare of all people. To those who regularly use it it begets joy and destroys every anxiety” (as cited in Grierson, 1894, p. 248).
Finally, in 1689 an account of the plant from India called Bangue, at that time largely unfamiliar to the British, was presented before the Royal Society. Descriptions of the effects upon ingesting a dose included:
…yet is he very merry, and laughs, and sings….after a little Time he falls asleep, and sleepeth very soundly and quietly; and when he wakes, he finds himself mightily refresh’d….it seemeth to put a Man into a Dream, or make him asleep, whilst yet he seems to be awake, but at last ends in a profound Sleep, which rectifies all. (Hooke, 1726, pp. 210, 212)
The Scientific Era
In the modern scientific era (i.e., mid 18th century onward), a new appreciation for and interest in the medical benefits and potential negative effects of cannabis developed. However, as far back as 1843 modern doctors used cannabis tincture successfully as an anxiolytic, soporific, and hypnotic for those suffering from morphine withdrawal symptoms, as well as a number of other ailments (e.g., Clendinning, 1843). Explorers and doctors from this era mention the effects of cannabis being at first stimulating, but then resulting in a “soft and pleasant drowsiness, from which I sank into a deep, refreshing sleep” (Taylor, 1855, p. 134). Others note cannabis as a remedy for “sleeplessness”, as a “calmative and hypnotic” (McMeens, 1860/1973, p. 135), and as a “moderate anodyne and soporific” (Clarke, 1878, p. 179) that results in “a prostration that is full of languor and charm” (Trousseau & Pidoux, 1880, p. 265).
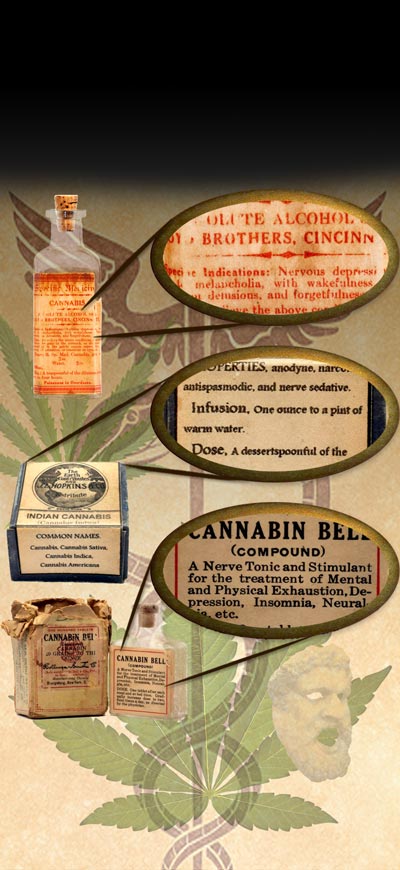
Starting in the late 1850s, hashish candy for medical purposes was regularly advertised in newspapers and magazines. For example, in the October 16th, 1858 edition of Harper’s Weekly, a small advertisement for Gunjah Wallah’s Hasheesh Candy promises the user “A most pleasurable and harmless stimulant – Cures Nervousness [emphasis added], Weakness, Melancholy &c. Inspires all classes with new life and energy” (reprinted in Ludlow, 1857/1975, p. 201). Other examples include similar advertisements in Vanity Fair from August 16, 1862 (“Antique cannabis medicines: Hasheesh candy”, 2010).
According to other reputable medical sources of the time, cannabis “is a useful adjuvant, in small doses, to other hypnotic remedies” (Lyman, 1885, p. 68) and “is well known as a sedative” (Mackenzie, 1887, p. 97). In addition, an advertisement in the May 5th, 1888 Cincinnati Lancet-Clinic for “Grimault’s Cigarettes of Cannabis Indica” mentions insomnia as one of the conditions that the cigarettes treat (“Grimault’s Cigarettes of Cannabis Indica”, p. 16). Others also noted that cannabis “sometimes impaired power of locomotion, the limbs feeling as if weighted with lead” (Stillé, Maisch, Caspari, & Maisch, 1894, p. 395), but then “produces sleep” (Pierce, 1895, p. 343). Dr. Mattison, writing in 1891 based on a decade of his own use of cannabis medications with his patients as well as the testimony of many other physicians of the time, including one who used cannabis as a hypnotic with 1000 patients (finding success in 530 and partial success in 215), concluded “cannabis indica is, often, a safe and successful anodyne and hypnotic” (Mattison, 1891/1973, p. 157).
Cannabis’ reputation to induce these effects continued unabated. It is listed as a “Sedative, anodyne, hypnotic” in Squire’s (1899, p. 179) Companion to the Latest Edition of the British Pharmacopoeia. In Merck’s 1899 Manual of the Materia Medica, a preparation made with cannabis extracts named Cannabine Tannate Merck is recommended as a “Hypnotic, Sedative” used for “[h]ysteria, delirium, [and] nervous insomnia” (“Cannabine Tannate Merck”, 1898, p. 26). Cushny (1906, p. 233) defines cannabis as a hypnotic in A Textbook of Pharmacology and Therapeutics and states; “…the symptoms eventually pass into tranquil sleep, from which he awakens refreshed, and, as a rule, without any feeling of depression or nausea”. In addition, the 1907 and 1930 Merck Indexes state that cannabis is a “Hypnotic; …Nervine; [and is] Sudorific…” (“Cannabis indica”, 1907, p. 123; “Cannabis”, 1930, p. 147)
In The Household Physician McGregor-Robertson (1907, p. 438) states “Indian hemp is used to relieve pain and produce sleep”, while Dock’s 1908 Textbook of Materia Medica for Nurses calls cannabis a hypnotic and asserts that it causes “a heavy sleep” (p. 241). Both of Squire’s 1908 (p. 315) and 1916 (p. 381) editions of Companion to the Latest Edition of the British Pharmacopoeia call cannabis a sedative, as does the 1925 edition of Lilly’s Handbook of Pharmacy and Therapeutics (“Cannabis”, 1925, p. 51). In addition, a Parke-Davis and Company physicians’ catalog from 1929-1930 lists cannabis as a sedative (reprinted in Mikuriya, 1973, p. 66). Furthermore, Blumgarten’s 1932 Textbook of Materia Medica also states that cannabis is used to “produce sleep” (p. 338).
Bruce and Dilling’s Materia Medica and Therapeutics states that – after cannabis prohibition began to spread around the Western world – cannabis was formerly used as a hypnotic that produced effects “ending in a stuporous sleep” (Dilling, 1933, p. 383), while The British Pharmaceutical Codex, 1934 still called cannabis a “sedative or hypnotic” (Pharmaceutical Society of Great Britain, 1934, p. 270). In 1934, Dr. Bromberg, a psychiatrist, also noted that “the smoker becomes drowsy, falls into a dreamless sleep and awakens with no physiological after effects” (as cited in Walton, 1938/1973, p. 112), and the editors of the 1935 book Everybody’s Family Doctor call cannabis a “sleep producing drug” (“Cannabis indica”, 1935, p. 130). Finally, in Solomon’s (1935, p. 205) Prescription Writing and Formulary, cannabis is listed as an ingredient in a sedative mixture.
Medical Indexes and Textbooks: Lying About the Risks but Telling the Truth About the High
While inaccurate about the risks of cannabis use, such as the claims that it causes schizophrenia, cancer, and violence (please refer to the free series of informative articles at www.stressedanddepressed.ca. for more in depth information), post-cannabis-prohibition medical textbooks, manuals, and indexes (in the U.S., post-1937) continued to tell the truth about the actual effects of proper cannabis use. For instance, cannabis is listed as a hypnotic and a sedative in the 1940 edition of the Merck Manual of Therapeutics and Materia Medica (“Cannabis”, 1940, p. 1356), and the pharmaceutical trade journal Ciba Symposia in 1946 (Robinson, 1946, p. 404) points out that cannabis “is sometimes employed as a hypnotic in those cases where opium, because of long-continued use, has lost its efficiency”. Furthermore, The Dispensatory of the United States of America of 1947 states that cannabis is used to “encourage sleep, and to soothe restlessness” (Osol & Farrar, 1947, p. 1383). A few years later, Solomon again affirmed cannabis “produces sleep” (1952, p. 189) in Pharmacology and Therapeutics. In 1959, Fishbein (p. 761) asserted that marihuana causes one to be “relaxed” and then to experience “drowsiness” in The Modern Family Health Guide.
But by the 1960s, many editors and writers of medical indexes and manuals distanced themselves from the current use of cannabis for medical purposes, and often employed phrases such as “…formerly [used] as analgesic and sedative” (e.g., Stecher, Finkel, & Siegmund, 1960, p. 204; Stecher, Windholz, & Leahy, 1968, p. 201; Wade & Reynolds, 1977, p. 298) – the word formerly in reference to the relatively newly instituted cannabis prohibition laws, rather than any noted change in cannabis’ actual effects. However, both the 1983 (Windholz, Budavari, Blumetti, & Otterbein, 1983, p. 1728) and the 2001 Merck Index (O’Neil et al., 2001, p. 292) continued to list drowsiness as an effect of cannabis smoking/inhalation.
Government Reports
Despite the preceding positive reports about the effects of cannabis, concerns about the potential negative effects of cannabis on the physical and mental well-being of its consumers and society have also been part of the historical records. Thus, due to the controversy surrounding the use of cannabis, several countries’ governments have commissioned large-scale reports, on multiple occasions, to investigate the impacts of cannabis use on society and individuals. These comprehensive studies date back to over 100 years, have each typically taken several years to complete, and have included panels of experts from every discipline of study conceivably impacted by the use of cannabis. From the first government-commissioned report in 1894 up to the present day, all have noted the anxiolytic and hypnotic effects of cannabis.
For example, in 1894 the British-initiated Indian Hemp Drugs Commission Report found sleep to be a well-known effect of the use of cannabis, noting “[t]he drug produces in some persons a curious loss of sense of space and time. This stage is generally followed by deep sleep…the intoxication lasts about three hours, when sleep supervenes” (Indian Hemp Drugs Commission, 1894, p. 193). Moreover, the Commission also noted “…slight narcotic effects, or stupor more or less complete” (p. 192). Fifty years later, the La Guardia Committee Report, the first in-depth investigation of smoked cannabis in the U.S., specifically looking at what was happening in New York, reported effects such as “…the subject generally lay on his bed and dozed or listened to the radio. His drowsiness persisted for many hours” (Mayor’s Committee on Marihuana, 1944, p. 129).
The British conducted their own investigation and in 1968 published what is commonly known as the Wootton Report, which “…found a large measure of agreement among witnesses about the principal subjective effects of the drug. Most gave chief emphasis to its relaxing and calming effect” (U.K. Home Office, 1968, p. 11). Canada soon followed, and in 1972 published what is commonly called the Le Dain Commission, which came to similar conclusions, reporting in the interim report of 1970 that “…it generally acts as a relaxant” (Le Dain, 1970, p. 202). Nearly simultaneously, president Richard Nixon commissioned a report to study cannabis abuse in the U.S., commonly referred to as the Shafer Commission, which reported that “[a]t low, usual ‘social’ doses, the intoxicated individual may experience…a dreamy, care-free state of relaxation” (Shafer, 1972, p. 68).
The Canadian Senate Special Committee on Illegal Drugs more recently reported that “[l]ow doses generally produce the effects that cause people to like smoking pot. They include mild euphoria, relaxation, increased sociability and a non-specific decrease in anxiety” (Nolin et al., 2002, p. 137). Thus, to date, every country that has commissioned an expertly conducted study of the effects of cannabis use has come to the same conclusion: Cannabis, when used at proper doses, has anxiolytic, hypnotic, relaxant, sedative, and soporific properties.
Cross-Cultural Use
Humans brought cannabis with them wherever they migrated (Robinson, 1996). Chopra and Chopra (1957) describe the indigenous use of cannabis in India, and among the uses is to relieve pain, to help with sleeping, to remove fatigue, and to calm restlessness. According to African people interviewed by ethnobotanists, dagga (cannabis) helps them to “forget all our troubles” (as cited in Andrews & Vinkenoog, 1968, p. 147). “In Jamaica….taken at bedtime, ganga [cannabis], is used to assure a good night’s sleep and waking refreshed” (Rubin, 1976, p. 9). In Thai folk medicine, “infusions of ganga are also taken before meals and sleep as a relaxant” (Rubin, 1976, p. 3), while cannabis is also listed in all official current Chinese pharmacopoeias as – among other things – a sedative (Rätsch, 1998/2001, p. 23), and finally, in Latin American folk medicine, cannabis “is smoked for sleep disorders and exhaustion” (Rätsch, 1998/2001, p. 150).
Recent Studies
Modern scientific studies continue to substantiate the observations of ancient cultures, while showing a more nuanced interaction between the consumer and the plant. For instance, after an extensive review of the then extant literature, Mikuriya (1969) made a list of the medical uses for cannabis, under the title of Possible Therapeutic Applications of Tetrahydrocannabinols and Like Products. The list included “Analgesic-hypnotic…Antidepressant-tranquilizer” (p. 39). But other research (e.g., both challenge and experience sampling studies) supports a role for cannabis in inducing anxiety in users (Holland, 2010); however, cannabis appears to increase anxiety in those already highly psychosis-prone in experience sampling studies (as cited in Holland, 2010), but not in a nonclinical population (Tournier, Sorbara, Gindre, Swendsen, & Verdoux, 2003). Other evidence points to THC, and particularly the dose of THC, being primarily responsible for anxiety responses experienced by some users (for a review of this literature, see Degroot, 2008 or Zuardi, Shirakawa, Finkelfarb, & Karniol, 1982).
Other studies suggest that novice users are more likely to have anxiety responses than those with experience. For instance, a study of 17 subjects at Duke University found that cannabis smoking increased anxiety in inexperienced users but decreased it in experienced ones (Mathew, Wilson, & Tant, 1989). However, in a follow-up study by Mathew, Wilson, Humphreys, Lowe, and Wiethe (1992), cannabis did not produce anxiety, even in infrequent users. The authors argue that this is likely because adverse effects are most often associated with novice users, and although the participants were infrequent users, they did have experience.
Hayatbakhsh et al. (2007) found an association between age of onset, level of use, and later anxiety, and it was strongest for those who initiated use before age 15. In addition, a recent meta-analysis of 83 studies found that for cannabis users, age at onset of first psychosis was younger than for nonusers (Large, Sharma, Compton, Slade, & Nielssen, 2011). However, it is important to note that at least one longitudinal study following participants from preschool through age 18 found that those who experimented with drug use during their adolescence (up to once a month, almost exclusively with cannabis), were the best adjusted, both psychologically and socially, compared to both frequent users and abstainers (Shedler & Block, 1990). It is also important to keep in mind that correlation does not equal causation. In fact, emerging evidence suggests that accounting for childhood traumas such as sexual abuse may diminish the association sometimes found between cannabis use and psychosis, and therefore, researchers investigating the association between cannabis use and psychiatric disorders should adjust their analyses to account for this potentially confounding variable (Houston, Murphy, Shevlin, & Adamson, 2011).
Moreover, reviews and meta-analyses of the existing literature cast doubt on the alleged causal role cannabis plays in the development of anxiety disorders. For example, in a recent review of the evidence for the potential role cannabis plays in the development of psychiatric disorders, the authors conclude that, “…taken together, the epidemiological evidence does not support a causative or precipitating role for cannabis in chronic depression or anxiety” (Fride & Russo, 2006, p. 376). Furthermore, a recent meta-analysis of prospective cohort studies, which controlled for potential confounding variables, also concluded that the evidence does not support a causal role for cannabis in anxiety or other affective disorders (Moore et al., 2007).
Interestingly, now that pharmaceutical companies are again actively involved in developing medicines derived from cannabis, evidence is mounting for the vast therapeutic potential of cannabis and the cannabinoids. For example, GW Pharmaceuticals’ research with their patented whole-plant extract buccal spray, Sativex®, also demonstrates the hypnotic potential of cannabinoids and cannabis. Russo, Guy, and Robinson (2007) first outline the history of the use of cannabis as a sleep aid and then review past clinical studies demonstrating the effects of various cannabinoids on sleep. Next, they present evidence from multiple Phase I – III clinical trials involving 2000 patients suffering from a wide variety of pain conditions and 1000 patient years of exposure, showing marked improvement in sleep with few adverse side effects. Moreover, the authors found:
[n]o tolerance to the benefit of Sativex on pain or sleep, nor need for dosage increases have been noted in safety extension studies of up to four years, wherein 40 – 50% of subjects attained good or very good sleep quality, a key source of disability in chronic pain syndromes that may contribute to patients’ quality of life. (p. 1729)
This is likely due to the ratios of the active compounds, as Sativex® contains a 1:1 ratio of ∆9-tetrahydrocannabinol (THC) to cannabidiol (CBD), THC being the primary psychoactive ingredient in cannabis and CBD being another important but nonpsychoactive cannabinoid that counters some of the unwanted effects of THC alone (McPartland & Russo, 2006; Russo, 2011; Russo et al., 2007). In fact, despite some research indicating that CBD alone helps improve sleep (e.g., Carlini & Cunha, 1981), it appears that CBD dominant extracts are mildly activating while THC dominant extracts leave residual sedative effects, and thus, the two compounds act synergistically, in the proper combination, to provide maximum benefits with the least adverse consequences (Russo et al., 2007).
Thus, researchers have identified the cannabinoids THC, CBD, and cannabichromene (CBC) as the primary sources of cannabis’ sedative (McPartland & Russo, 2006; Rätsch, 1998/2001; Russo et al., 2007), anxiolytic, and antipsychotic effects (Degroot, 2008; Zuardi, Crippa, Hallak, Moreira, & Guimaraes, 2006; Zuardi & Guimaraes, 1997). For instance, a study of healthy normal subjects with induced anxiety found that anxiety was reduced by CBD alone (Zuardi, Cosme, Graeff, & Guimaraes, 1993). In fact, Degroot (2008) provides a table of 12 preclinical and clinical studies, all showing that CBD produces anxiolytic effects. Furthermore, in addition to resolving THC induced anxiety, CBD also mitigates many of the other negative effects associated with THC, such as cognitive impairment (Russo et al., 2007; Zuardi et al., 1982).
Further evidence comes from studies with people suffering from psychosis and/or schizophrenia. This is important for this discussion because of the very high levels of anxiety, agitation, and stress that are often caused by the more dramatic symptoms of psychosis and/or schizophrenia, and therefore, a reduction in psychotic symptoms also leads to a reduction in anxiety and stress. For instance, a study of 79 psychotics found that those who used cannabis recreationally reported less anxiety, depression, insomnia, and physical discomfort than those who did not use cannabis (Warner et al., 1994), and a phase II clinical trial on the effects of CBD in schizophrenia and schizophreniform psychosis revealed that CBD was as effective as amisulpride, a standard antipsychotic in Europe and Australia and available in Canada through the Special Access Program but not available in the United States, in reducing acute psychosis symptoms, but with far fewer negative side effects (Canadian Agency for Drugs and Technologies in Health, 2011; Kaplan, 2004; Lecrubier et al., 2001; Leweke et al., 2005). Other studies substantiate these findings (e.g., Zuardi et al., 2006; Zuardi & Guimaraes, 1997).
Corroborative support for the anxiolytic and hypnotic, soporific, and sedative effects of cannabis and the cannabinoids comes from a surprising source. In 2007, rimonabant, a CB1 receptor blocker developed as an anti-obesity drug by French company Sanofi-Aventis under the trade name Acomplia®, was denied Food and Drug Administration (FDA) approval by the U.S. because it was linked to increased depression, suicidal thoughts, suicide attempts, suicide events, anxiety [emphasis added], and insomnia [emphasis added] (Badawi, n.d.; Gieringer et al., 2008). Considering the evidence strongly suggesting the anxiolytic and hypnotic effects of cannabis, as well as the known mechanisms of action of the cannabinoids and the homeostatic role the endocannabinoid system plays, it should not be surprising that blocking one of the main receptors for the cannabinoids would lead to these adverse events.
Of particular importance in this discussion is the fact that the federal Medical Marihuana Access Regulations in Canada already allow for the use of cannabis for anxiety and severe stress, among other psychiatric conditions, as well as sleep disorders, so long as the appropriate form (i.e., Form B2) is completed by a qualified medical professional (Health Canada, 2005, 2007). The situation in the United States is a little bit more complicated because they do not have a federal medical cannabis program. However, to date sixteen states and the District of Columbia have enacted their own laws to legalize cannabis for medical purposes, and of those, thirteen leave room for the use of cannabis for anxiety and/or other psychiatric conditions by including medical conditions whose primary symptoms include anxiety, such as Post Traumatic Stress Disorder, by allowing the use of cannabis for any chronic or persistent medical condition that limits a person’s ability to perform one or more major life activities or if not alleviated, could cause serious mental or physical harm to the patient, or by allowing the use of cannabis for any number of unspecified medical conditions upon the approval of the various state Departments of Health (California Senate Bill 420, 2003; ProCon.org, 2011).
However, despite the evidence and both federal and state programs allowing for the use of cannabis for anxiety, it is acknowledged that treating anxiety “…with cannabis may be difficult because of differences in individual makeup, need for continuous dose levels, expense, availability, and illegality” (Mikuriya, 1998).
Comparisons With Synthetic Medicines
Lester Grinspoon, retired Harvard Medical professor and world-renowned cannabis expert who specialized in the study and treatment of schizophrenia, reported that in clinical practice cannabis and cannabinoids compare favorably in both efficacy and safety to many pharmaceutical antianxiety medications (Grinspoon & Bakalar, 1993). Moreover, numerous independent assessments of the safety, efficacy, and dependence potential of cannabis clearly indicate that cannabis and cannabis-based medications are well-tolerated, non-toxic, cannot lead to death by overdose, and are unlikely to lead to dependence in the vast majority of patients. For instance, the Institute of Medicine’s 1999 report, Marijuana and Medicine: Assessing the Science Base, in relation to the safety of cannabis, noted: “The side effects of cannabinoid drugs are within the acceptable risks associated with approved medications” (Joy, Watson, & Benson, 1999, p. 127). In addition, in 1988 the Drug Enforcement Agency’s Chief Administrative Law Judge, Francis Young, after two years of hearing expert testimony and reviewing thousands of documents concluded:
A smoker would theoretically have to consume nearly 1,500 pounds of marijuana within about 15 minutes to induce a lethal response. In practical terms, marijuana cannot induce a lethal response as a result of drug-related toxicity….In strict medical terms marijuana is far safer than many foods we commonly consume. For example, eating 10 raw potatoes can result in a toxic response. By comparison, it is physically impossible to eat enough marijuana to induce death. Marijuana in its natural form is one of the safest therapeutically active substances known to man. By any measure of rational analysis marijuana can be safely used within the supervised routine of medical care. (Young, 1988, pp. 57-59)
In addition, studies comparing cannabinoids to pharmaceuticals have shown that they often offer therapeutic equivalence to pharmaceuticals, with fewer negative side effects. For instance, in an experiment with college students in a public-speaking model of anxiety, compared with placebo CBD achieved significant improvement in subjective anxiety equivalent to Valium and ipsapirone (Zuardi & Guimaraes, 1997). Moreover, as previously mentioned, CBD was as effective as amisulpride, a standard antipsychotic, in reducing acute psychosis symptoms, but with far fewer negative side effects (Leweke et al., 2005).
Sadly, the same safety and efficacy profile cannot be said to exist for many of the conventional pharmaceutical medications used to treat anxiety and sleeping problems, with well-known court cases and science establishing the very real and potentially dangerous side-effects of drugs like the commonly prescribed Serotonin Specific Reuptake Inhibitors (SSRIs) (Degroot, 2008; Kauffman, 2009). For instance, it is well established that during the early stages of treatment with SSRIs that anxiety is actually likely to increase, and that certain populations are at increased risk of suicide or self-harm (Degroot, 2008; Kauffman, 2009). As a result, to reduce these potential side effects, early treatment with SSRIs is often combined with the use of drugs like benzodiazapines (which have a list of their own serious negative side effects) (Degroot, 2008; Longo & Johnson, 2000). Furthermore, along with a host of physical and psychological complaints (Degroot, 2008; Kauffman, 2009), the potential side effects of SSRIs may include homicide and suicide (Kauffman, 2009). In fact, case precedence has established that murder and suicide are potential side effects of SSRI use and the manufacturer can be, and has been, held liable (Kauffman, 2009; see http://ssristories.com/index.php for a list of violent incidents and court cases associated with SSRI use). Neither of these outcomes has been shown to be causally associated with the use of cannabis (Price, Hemmingsson, Lewis, Zammit, & Allebeck, 2009; Reiss & Roth, 1993).
Because anxiety often accompanies depression and SSRIs are commonly used to treat both conditions, the problems outlined above (e.g., increased anxiety, suicide, and self-harm) may be compounded. It may very well be that millions of patients are not only being prescribed a more dangerous medication than cannabis, but also that most of them are deriving no benefit while shouldering substantial risks. For example, Kirsch, Moore, Scoboria, and Nicholls (2002) analyzed both published and unpublished clinical trials submitted to the U.S. FDA on the six most commonly prescribed SSRIs and found that placebo control groups duplicated about 80% of the response to medication. In 2008, Kirsch et al. conducted a meta-analysis on data submitted to the FDA on four new-generation antidepressant medications. They found that the medications were ineffective in treating patients with moderate and even severe depression, with only minor clinical improvements in the most severely depressed.
It is important to note that emerging evidence demonstrates that many patients are turning to cannabis to safely and effectively reduce and/or replace synthetic antianxiety, hypnotic, soporific, and sedative medications after having grown tired of the negative side effects associated with their use. For example, many cannabis buyers club members say they use cannabis as a substitute for prescription narcotics (Gieringer, 1996), and in examinations of 2,480 California patients, Dr. Mikuriya found that 27% reported using cannabis for “mood disorders” and another 5% used cannabis as a substitute for more toxic drugs (Gieringer, 2002). Moreover, a recent survey of doctors in California found “that many of their patients were able to decrease their use of…antidepressant, anti-anxiety, and sleeping medications, or else they use cannabis to treat their side effects of jitteriness or gastrointestinal problems in order to stay on their medications” (Holland, 2010, p. 285). Currently, the most comprehensive study ever conducted in Canada investigating the barriers medical cannabis users encounter while trying to gain access to their medication of choice is underway (see https://www.surveymonkey.com/s/CannabisSurvey). The survey includes several questions about cannabis as a substitute for both illicit drugs and prescribed pharmaceuticals.
Cannabis as Preventive Medicine
Those studying the plant and its uses throughout world cultures, as well as human history, have observed the ability of cannabis and the cannabinoids to prevent illness, and not just treat symptoms, for some time. For instance, in 1845 in relation to the use of hashish and its effects, Moreau wrote, “I report them here only to call attention to the prophylactic action [emphasis added] of a substance that could offer valuable therapeutic resources” (Moreau, 1845/1973, p. 213).
More recently, after an extensive review of the then extant literature, Mikuriya (1969) made a list of the medical uses for cannabis, under the title of Possible Therapeutic Applications of Tetrahydrocannabinols and Like Products. The list included “Prophylactic [emphasis added] and treatment of the neuralgias, including migraine and tic douloureux” (p. 39). Even more recently, in an interview about her research into prenatal exposure to cannabis and neonatal outcomes in Jamaica, Dr. Dreher, nurse, anthropologist, and current dean of nursing at Rush University Medical Centre, had the following to say about the importance of cultural context and the preventive properties of cannabis:
American drug use often takes place without cultural rules and in an unsupervised context. The Jamaican women we studied had been educated in a cultural tradition of using marijuana as a medicine. They prepared it with teas, milk and spices, and thought of it as a preventive and curative substance [emphasis added].…Some of these women were in dire socioeconomic straits, and they found that smoking ganja helped allay feelings of worry and depression [emphasis added] about their financial situation. (Brady, 1998)
Rätsch (1998/2001), writing about the use of cannabis in Jamaica amongst Rastafarians noted that:
[h]emp tea is a popular drink for preventive use [emphasis added] and is also consumed therapeutically for almost all ailments. Hemp preparations are often ingested for prophylactic purposes [emphasis added]. The frequent use does not just protect from diseases, but also gives courage and strength… (p. 140)
It is important to note that one can also infer the preventive medicine properties of cannabis by taking a step back and, instead of focusing on one or two narrow medical conditions for which cannabis may be used, recognizing the sheer volume of and widely disparate chronic and acute medical conditions and/or symptoms for which cannabis has already been proven effective in treating, for which accumulating evidence strongly suggests cannabis is effective in treating, and for which preliminary research shows cannabis is potentially effective in treating. These varied and serious medical conditions and symptoms include, but are not limited to, nausea and vomiting, wasting syndromes associated with AIDS and cancer, multiple sclerosis, amyotrophic lateral sclerosis, spinal cord diseases and injuries, epilepsy and other seizure disorders, a variety of chronic pain conditions (e.g., migraine, fibromyalgia, rheumatoid arthritis, neuropathy), a variety of movement disorders, glaucoma, a variety of psychiatric disorders, a variety of inflammatory diseases, and various cancers (e.g., Fride & Russo, 2006; Grinspoon, Bakalar, & Russo, 2005; Guzmán, 2003; Health Canada, 2010; Russo, 2001). A rational analysis of the body of evidence demonstrating the ability of a single substance, cannabis, to treat or potentially treat such a wide variety of medical conditions and symptoms through its actions on the endocannabinoid system, which acts as a bodily homeostatic regulator, very strongly suggests that cannabis likely plays a role in delaying the progression of and/or preventing many illnesses when used properly.
However, perhaps the most powerful evidence of the preventive properties of cannabis and the cannabinoids comes from the U.S. government itself. In 2003 the government, as represented by the Department of Health and Human Services, was awarded patent number 6630507, entitled Cannabinoids as Antioxidants and Neuroprotectants. The abstract states, in part, that cannabinoids are “…useful in the treatment and prophylaxis [emphasis added] of wide variety of oxidation associated diseases, such as ischemic, age-related, inflammatory and autoimmune diseases” (Hampson, Axelrod, & Grimaldi, 2003, Abstract section).
Beginning to Understand the Nuances of Cannabis Medicine
Cannabis has paradoxical effects, having for instance both relaxing and stimulating effects. However, these effects are based upon many factors, including the strain of cannabis, the quality, potency, and purity of the strain, number of types and ratios of cannabinoids, number of types and ratios of terpenes (compounds that produce the unique aromas and tastes of individual strains, but which have their own proven therapeutic properties and which act synergistically with the cannabinoids), dose, and the health, setting, mindset, and diet of the user, as well as the user’s experience with and tolerance to the various cannabinoids (e.g., Gieringer et al., 2008; McPartland & Russo, 2006; Russo, 2011).
These factors, influencing the effects of cannabis upon its consumers, have been known for quite some time. For instance, in The National Dispensatory of 1894 it is written that “the plants richest in resin grow at an altitude of 1800 to 2400 m” (Stillé et al., p. 393) and that the effect of cannabis “varies with the individual’s temperament” (Stillé et al., p. 395). In Cushny’s 1906 Pharmacology and Therapeutics or the Actions of Drugs the effects of cannabis are described as:
…a mixture of depression and stimulation…its action…seems to depend very largely on the disposition and intellectual activity of the individual. The preparations used also vary considerably in strength, and the activity of even the crude drug seems to depend very largely on the climate and season in which it is grown, so that great discrepancies occur in the account of its effects. (p. 232)
One text notes that “[p]reparations made from plants grown in warm climates are usually better” (Blumgarten, 1932, p. 338). Another notes that after two years of storage “…it had lost about half its potency” (Osol & Farrar, 1947, p. 1382). Still another notes that “[m]any of the psychological effects seem related to the setting in which the drug is taken” (Holvey et al., 1972, p. 1415). One even noted “…an occasional panic reaction has occurred, particularly in naive [sic] users, but these have become unusual as the culture has gained increasing familiarity with the drug” (Berkow et al., 1982, p. 1427). Another noted that cannabis’ effects are dependent upon “the dose of the drug and the underlying psychological conditions of the user” (Venes et al., 2001b, p. 1242).
Unfortunately, the prohibition of cannabis had a negative effect on its medicinal reputation. Textbooks began to remark upon the “completely unpredictable” nature of the drug (Faddis, 1943, p. 153) or its unreliability in providing consistent results (“Cannabis”, 1952; Dilling, 1933) – blaming the drug itself for the researchers’ and cultivators’ lack of understanding of the proper cultivation, storage, and transportation of cannabis for medicine, as well as of the various strains, the strains’ types and ratios of cannabinoids and the effects of each on the user, and of the importance of the subject’s mindset and setting within which cannabis is consumed. Some textbooks then began omitting entirely any mention of cannabis in their later editions (e.g., Blumgarten, 1940; Pierce, 1935). Others began to falsely blame whole-plant cannabis for the effects experienced by one of its isolated, synthesized, and concentrated cannabinoids, particularly THC (Gieringer et al., 2008; Wade & Reynolds, 1977). This is of particular importance because the evidence is mounting that several cannabinoids, as well as the terpenoids and flavonoids present in whole-cannabis, are important, and they act synergistically to enhance some of the positive effects and to reduce some of the negative effects of cannabis use, such as the cognitive impairment associated with THC (e.g., McPartland & Russo, 2006; Russo, 2011; Russo & Guy, 2006; Russo et al., 2007).
Still, the special relationship between cannabis’ prohibition and its reputation as a dangerous or unpredictable drug was accurately assessed in the 1987 Merck Manual of Diagnosis and Therapy: “…the chief opposition to the drug rests on a moral and political, and not a toxicological, foundation” (Berkow et al., 1987, p. 1490). The numerous studies and commissioned reports conducted since 1987, some of which call for the outright legalization and regulation of cannabis (e.g., Senate Special Committee on Illegal Drugs of 2002), but which have been ignored, only reinforce this conclusion.
What About the Smoke?
We understand that many health-care professionals are reluctant to recommend cannabis to their patients due to the potential pulmonary damage from smoking whole cannabis. However, despite what many believe about harms associated with smoking cannabis, the best available evidence strongly suggests that it does not lead to lung cancer. In fact, the evidence strongly suggests that the cannabinoids offer a protective factor against the development of several kinds of cancer (see for example Guzmán, 2003). For more detailed information about this topic, as well as other cannabis myths, please refer to the free series of informative articles at www.stressedanddepressed.ca.
That being said, the harms associated with smoking cannabis can be mitigated or eliminated through harm reduction techniques such as vaporizing or ingesting cannabis (see for example Earleywine & Van Dam, 2010). For more detailed information about this, please refer to the free series of informative articles at www.stressedanddepressed.ca.
Conclusion
When all the evidence is considered together and taken in context, it is clear that cannabis has been used safely and effectively as a stress and anxiety-reliever, as a sedative, and as an aid to sleep for thousands of years, continues to be used for those purposes by many cultures all over the world, and modern science corroborates those uses, when used properly. Therefore, if, after reviewing the evidence surrounding its safety, cannabis is found to pose an acceptable risk for medical use, it should be considered by physicians as a legitimate treatment option for those who are currently dealing with anxiety, stress, and/or insomnia, as well as for those who wish to avoid – or, in the case of current users, continue to avoid – these serious conditions.
References
American Psychological Association (APA). (n.d.). Anxiety. Retrieved November 24, 2011 from http://www.apa.org/topics/anxiety/index.aspx
Andrews, G., & Vinkenoog, S. (Eds.). (1968). The book of grass: An anthology on Indian hemp. New York: Grove Press.
Antique cannabis medicines: Hasheesh candy. (2010, October). In The antique cannabis book. Retrieved November 18, 2011 from http://antiquecannabisbook.com/chap15/QCandy.html
Badawi, O. (n.d.). Cardiovascular disorders: Rimonabant trial halted early because of suicide risk. Retrieved November 16, 2011 from American Pharmacists Association website http://www.pharmacist.com/AM/Template.cfm?Section=Pharmacy_News &template=/CM/ContentDisplay.cfm&ContentID=24206
Berkow, R., et al. (Eds.). (1982). Drug dependence: Dependence of the cannabis (marijuana) type. In The Merck manual of diagnosis and therapy (14th ed., pp. 1426-1427). Rahway, NJ: Merck & Co., Inc.
Berkow, R., et al. (Eds.) (1987). Drug dependence: Dependence of the cannabis (marijuana) type. In The Merck manual of diagnosis and therapy (15th ed., pp. 1476-1495). Rahway, NJ: Merck & Co., Inc.
Blumgarten, A. S. (1932). Cannabis or cannabis indica (Indian hemp). In Textbook of materia medica (5th ed., pp. 338-339). New York: MacMillan Co..
Blumgarten, A. S. (1940). Textbook of materia medica, pharmacology and therapeutics (7th ed., rev.). New York: The MacMillan Co.
Brady, P. (1998, November 1). Dr. Melanie Dreher, reefer researcher. Retrieved November 15, 2011 from http://www.cannabisculture.com/articles/1404.html
Burton, R. F. (Trans.). (2003). Book of a thousand nights and a night, part 2. Whitefish, MT: Kessinger Publishing, LLC. (Original work published 1706).
California Senate Bill 420. (2003, February 20). California senate bill number: SB 420 – Bill text. Retrieved January 28, 2012 from http://medicalmarijuana.procon.org/sourcefiles/SB420.pdf
Canadian Agency for Drugs and Technologies in Health (CADTH). (2011, June 3). Amisulpride for
adults with refractory schizophrenia: A review of the clinical effectiveness and safety. Ottawa: Canadian Agency for Drugs and Technologies in Health. Retrieved January 29, 2012 from http://www.cadth.ca/media/pdf/htis/june-2011/RC0276_Amisulpride_for_Adults_with_Refractory_Schizophrenia_Final.pdf
Cannabine Tannate Merck. (1898). In Merck’s 1899 manual of the materia medica together with a summary of therapeutic indications and a classification of medicaments. A ready-reference pocket book for the physician and surgeon (p. 26). New York: Merck & Co.
Cannabis. (1925). In Handbook of pharmacy and therapeutics Lilly (7th Rev. ed., p. 51). New York: Eli Lilly and Company.
Cannabis. (1930). In Merck’s index. An encyclopedia for the chemist, pharmacist and physician (4th ed., p. 147). Rahway, NJ: Merck & Co., Inc.
Cannabis. (1940). In The Merck manual of therapeutics and material medica. A source of ready reference for the physician (7th ed., p. 1356). Rahway, NJ: Merck & Co., Inc.
Cannabis. (1952). In The Merck index of chemicals and drugs. An encyclopedia for the chemist, pharmacist, physician, and allied professions (6th ed., p. 196). Rahway, NJ: Merck & Co., Inc.
Cannabis indica. (1907). In Merck’s 1907 index. An encyclopedia for the chemist pharmacist and physicians (3rd ed., p. 123). New York: Merck & Co.
Cannabis indica. (1935). In Everybody’s family doctor (pp. 129-130). London: Odhams Press Ltd.
Carlini, E. A., & Cunha, J. M. (1981). Hypnotic and antiepileptic effects of cannabidiol. Journal of Clinical Pharmacology, 21, 4175-4275.
Chopra, I. C., & Chopra, R. W. (1957). The use of the cannabis drugs in India. Bulletin on Narcotics, 9, 4-29. Retrieved November 14, 2011 from http://multimedia.unodc.org/unodc/en/data-and-analysis/bulletin/bulletin_1957-01-01_1_page003.html
Clarke, E. (1878). Visions – A study of false sight (pseudopia). Boston: Houghton, Osgood and Company.
Clendinning, J. (1843). Observations on the medicinal properties of the cannabis sativa of India. Medico-Chirurgical Transactions, 26, 188-210.
Cohen, S., Janicki-Deverts, D., & Miller, G. E. (2007). Psychological stress and disease. Journal of the American Medical Association, 298(14), 1685-1687. doi:10.1001/jama.298.14.1685
Cushny, A. (1906). Cannabis indica. In A textbook of pharmacology and therapeutics or the actions of drugs in health and disease (4th ed., pp. 232-234). New York: Lea Brothers & Co..
Da Orta, G. (1895). Colloquies on the simples & drugs of India (C. De Ficalho, Ed., C. Markham, Trans.). London: Henry Sotheran and Co. (Original work published 1563). Retrieved November 26, 2011 from http://www.archive.org/stream/colloquiesonsimp00orta#page/n7/mode/2up
de Fonseca, F. R., Del Arco, I., Bermudez-Silva, F. J., Bilbao, A., Cippitelli, A., & Navarro, M. (2005). The endocannabinoid system: Physiology and pharmacology. Alcohol & Alcoholism, 40(1), 2–14. doi:10.1093/alcalc/agh410
Degroot, A. (2008). Role of cannabinoid receptors in anxiety disorders. In A. Köfalvi (Ed.), Cannabinoids and the brain (pp. 559-572). New York: Springer.
Dilling, W. J. (1933). Cannabis indica. In Bruce and Dilling’s materia medica and therapeutics an introduction to the rational treatment of disease (14th Rev. ed., p. 383). London: Cassell and Company, Limited.
Dock, L. L. (1908). The vegetable kingdom: Cannabis indica (Indian Hemp). In Text-book of materia medica for nurses (4th Rev. ed., pp. 241-242). New York and London: G. P. Putnam’s Sons.
Dorland, W. A. N. (1903a). Soporific. In The American illustrated medical dictionary: A new and complete dictionary (3rd ed., p. 635). Philadelphia: W. B. Saunders Company.
Dorland, W. A. N. (1903b). Hypnotic. In The American illustrated medical dictionary: A new and complete dictionary (3rd ed., p. 327). Philadelphia: W. B. Saunders Company.
Dorland, W. A. N. (1903c). Relaxant. In The American illustrated medical dictionary: A new and complete dictionary (3rd ed., p. 587). Philadelphia: W. B. Saunders Company.
Dorland, W. A. N. (1903d). Nervine. In The American illustrated medical dictionary: A new and complete dictionary (3rd ed., p. 457). Philadelphia: W. B. Saunders Company.
Dorland, W. A. N. (1903e). Sedative. In The American illustrated medical dictionary: A new and complete dictionary (3rd ed., p. 615). Philadelphia: W. B. Saunders Company.
Dorland, W. A. N. (1903f). Cerebral sedative. In The American illustrated medical dictionary: A new and complete dictionary (3rd ed., p. 615). Philadelphia: W. B. Saunders Company.
Dorland, W. A. N. (1903g). Narcotic. In The American illustrated medical dictionary: A new and complete dictionary (3rd ed., p. 445). Philadelphia: W. B. Saunders Company.
Dorland, W. A. N. (1960). Narcotic. In Dorland’s pocket medical dictionary (20th ed., p. N-1). Philadelphia: W. B. Saunders Company.
Earleywine, M., & Van Dam, N. T. (2010). Case studies in cannabis vaporization. Addiction Research and Theory, 18(3), 243-249.
El-Alfy, A. T., Ivey, K., Robinson, K., Ahmed, S., Radwan, M., Slade, D., et al. (2010). Antidepressant-like effect of delta9-tetrahydrocannabinol and other cannabinoids isolated from cannabis sativa l. Pharmacology Biochemistry and Behavior, 95(4), 434-442.
Faddis, M. O. (1943). Cerebrospinal depressants: Cannabis. In Textbook of pharmacology for nurses (2nd ed., p. 153). London: J. B. Lippincott Company.
Fishbein, M. (Ed.). (1959). Marihuana. In The modern family health guide: Encyclopedia of family health (Vol. 2, p. 761). Garden City, NY: Doubleday & Company, Inc.
Fride, E., & Russo, E. B. (2006). Neuropsychiatry: Schizophrenia, depression, and anxiety. In E. S. Onaivi, T. Sugiura, & V. Di Marzo (Eds.), Endocannabinoids: The brain and body’s marijuana and beyond (pp. 371-382). Boca Raton, FL: Taylor & Francis.
Glanze, W. D., Anderson, K. N., & Anderson, L. E. (Eds.) (1987a). Stress reaction. In The Signet-Mosby medical encyclopedia (p. 547). New York, NY: Penguin Books.
Glanze, W. D., Anderson, K. N., & Anderson, L. E. (Eds.) (1987b). Anxiety. In The Signet-Mosby medical encyclopedia (p. 39). New York, NY: Penguin Books.
Glanze, W. D., Anderson, K. N., & Anderson, L. E. (Eds.) (1987c). Narcotic. In The Signet-Mosby medical encyclopedia (p. 395). New York, NY: Penguin Books.
Gieringer, D. H. (1996). Review of human studies on medical use of marijuana. California: California NORML.
Gieringer, D. (2002). Medical use of cannabis: Experience in California. In F. Grotenhermen & E. Russo (Eds.), Cannabis and cannabinoids: Pharmacology, toxicology, and therapeutic potential (pp. 143-152). Binghamton, NY: The Hawthorn Press, Inc.
Gieringer, D., Rosenthal, E., & Carter, G. (2008). Marijuana medical handbook: Practical guide to the therapeutic uses of marijuana (2nd ed.). Oakland, CA: Quick American.
Grierson, G. A. (1894). Note by Mr. G. A. Grierson, C. I. E., magistrate and collector, Howrah, on references to the hemp plant occurring in Sanskrit and Hindi literature. In Report of the Indian Hemp Drugs Commission Report, 1893-94 (Vol. 3, pp. 246-249). Simla, India: The Government Central Printing Office. Retrieved November 29, 2011 from http://digital.nls.uk/indiapapers/browse/pageturner.cfm?id=74552210
Grimault’s Cigarettes of Cannabis Indica. (1888, May 5). Cincinnati Lancet-Clinic,16.
Grinspoon, L., & Bakalar, J. B. (1993). Depression and other mood disorders. In Marijuana, the forbidden medicine (pp. 115-126). New Haven: Yale University Press.
Grinspoon, L., Bakalar, J. G., & Russo, E. (2005). Marihuana: Clinical aspects. In J. H. Lowinson, P. Ruiz, R. B. Millman, & J. G. Langrod (Eds.), Substance abuse: A comprehensive textbook (4th ed., pp. 263-276). Baltimore: Lippincott Williams & Wilkins.
Grotenhermen, F. (2006a). Mini-review: Cannabinoids and the endocannabinoid system. Cannabinoids, 1(1), 10-14.
Grotenhermen, F. (2006b). Clinical pharmacodynamics of cannabinoids. In E. B. Russo & F. Grotenhermen (Eds.), Handbook of cannabis therapeutics from bench to bedside (pp. 117-170). New York: Taylor and Francis Group.
Guzmán, M. (2003). Cannabinoids: Potential anticancer agents. Nature Reviews, 3, 745-755.
Guzmán, M. (2005). Effects on cell viability. In R. G. Pertwee (Ed.), Cannabinoids: Handbook of experimental pharmacology, 168 (pp. 627-642). Heidelberg: Springer-Verlag.
Hampson, A. J., Axelrod, J., & Grimaldi, M. (2003). U.S. Patent No. 6,630,507. Cannabinoids as antioxidants and neuroprotectants. Retrieved November 15, 2011 from http://www.patentstorm.us/patents/6630507.html
Hayatbakhsh, M. R., Najman, J. M., Jamrozik, K., Mamun, A. A., Alati, R., & Bor, W. (2007). Cannabis and anxiety and depression in young adults: A large prospective study. J. Am. Acad. Child Adolesc. Psychiatry, 46, 408-417.
Health Canada. (2005, last modified June). Frequently asked questions – Medical use of marihuana: Who is eligible to obtain an authorization to possess marihuana? Retrieved January 28, 2012 from http://www.hc-sc.gc.ca/dhp-mps/marihuana/about-apropos/faq-eng.php/#a3
Health Canada. (2007, revised). Form B2: Medical practitioner’s form for Category 2 applicants. Ottawa: Health Canada. Retrieved January 28, 2012 from http://www.hc-sc.gc.ca/dhp-mps/alt_formats/hecs-sesc/pdf/marihuana/how-comment/applicant-demandeur/form_b2-eng.pdf
Health Canada. (2010, September). Information for health care professionals: Marihuana (marijuana, cannabis). Ottawa: Health Canada. Retrieved January 29, 2012 from http://www.hc-sc.gc.ca/dhp-mps/alt_formats/hecs-sesc/pdf/marihuana/how-comment/medpract/infoprof/marijuana-monograph-eng.pdf
Hoerr, N. L., & Osol, A. (Eds.) (1952). Stress. In Blakiston’s illustrated pocket medical dictionary (p. 697). New York: McGraw-Hill Book Company, Inc.
Holland, J. (2010). Cannabinoids and psychiatry. In J. Holland (Ed.), The pot book: A complete guide to cannabis its role in medicine, politics, science, and culture (pp. 282-294). Rochester, VT: Park Street Press.
Holvey, D. N., et al. (Eds.). (1972). Drug dependence: Marihuana. In The Merck manual of diagnosis and therapy (12th ed., pp. 1414-1415). Rahway, NJ: Merck & Co., Inc.
Hooke, R. (1726). An account of the plant, call’d Bangue, before the Royal Society, Dec. 18. 1689. In W. Derham (Ed.) Philosophical experiments and observations of the late eminent Dr. Robert Hooke, S. R. S. and geom. prof. Grelb and other eminent virtuoso’s in his time (pp. 210-212). London: W. Derham. Retrieved December 8, 2011 from http://books.google.ca/books?id=t1sUAAAAQAAJ&printsec=frontcover#v=onepage&q&f=false
Houston, J. E., Murphy, J., Shevlin, M., & Adamson, G. (2011). Cannabis use and psychosis: Re-visiting the role of childhood trauma [Abstract]. Psychological Medicine, 41(11), 2339-2348.
Indian Hemp Drugs Commission. (1894). Report of the Indian Hemp Drugs Commission, 1893-94 (Vol. 1). Simla, India: The Government Central Printing Office. Retrieved November 29, 2011 from http://digital.nls.uk/indiapapers/browse/pageturner.cfm?id=74574070
Joy, J. E., Watson, S. J. Jr., & Benson, J. A. Jr. (Eds.). (1999). Marijuana and medicine: Assessing the science base. Washington, DC: National Academy Press.
Kaplan, A. (2004). Psychotropic medications around the world. Psychiatric Times, 21(5). Retrieved January 29, 2012 from http://www.psychiatrictimes.com/display/article/10168/47711#.
Kauffman, J. M. (2009). Selective serotonin reuptake inhibitor (SSRI) drugs: More risks than benefits? Journal of American Physicians and Surgeons, 14(1), 7-12.
Kirsch, I., Deacon, B. J., Huedo-Medina, T. B., Scoboria, A., Moore, T. J., & Johnson, B. T. (2008). Initial severity and antidepressant benefits: A meta-analysis of data submitted to the Food and Drug Administration. PLoS Med 5(2): e45. doi:10.1371/journal.pmed.0050045
Kirsch, I., Moore, T. J., Scoboria, A., & Nicholls, S. (2002). The emperor’s new drugs: An analysis of antidepressant medication data submitted to the U.S. Food and Drug Administration. Prevention and Treatment, 5(23), 1-11.
Large, M., Sharma, S., Compton, M. T., Slade, T., & Nielssen, O. (2011). Cannabis use and earlier onset of psychosis: A systematic meta-analysis [Abstract]. Archives of General Psychiatry, 68(6), 555-561. doi:10.1001/archgenpsychiatry.2011.5
Lecrubier, Y., et al. (2001). Consensus on the practical use of amisulpride, an atypical antipsychotic, in
the treatment of schizophrenia. Neuropsychobiology, 44(1), 41–46. doi:10.1159/000054913.
Le Dain, G. (1970). Interim report of the Commission of Inquiry into the non-medical use of drugs. Ottawa, ON: Information Canada.
Leweke, F. M., Koethe, D., Gerth, C. W., Nolden, B. M., Schreibe, D., Hänsel, A., et al. (2005). Cannabidiol as an antipsychotic: A double-blind, controlled clinical trial on cannabidiol vs amisulpride in acute schizophrenics. 2005 Symposium on the Cannabinoids, Burlington, VT, International Cannabinoid Research Society. Retrieved December 8, 2011 from http://CannabinoidSociety.org.
Li Shih-Chen. (1911). Cannabis sativa. In G. A. Stuart & F. P. Smith (Trans.), Chinese materia medica: Vegetable kingdom (pp. 90-91). Shanghai: American Presbyterian Mission Press. (Original work published 1593). Retrieved November 26, 2011 from http://www.archive.org/stream/chinesemateriame00stuauoft#page/90/mode/2up
Longo, L. P., & Johnson, B. (2000, April). Addiction: Part I. Benzodiazepines – side effects, abuse risk and alternatives. American Family Physician, 61(7), 2121–2128.
Ludlow, F. H. (1975). The hasheesh eater. The Fitz Hugh Ludlow memorial library edition (M. Horowitz, Ed.). San Francisco, CA: Level Press. (Original work published 1857).
Lyman, H. (1885). Remedies for insomnia. In Insomnia; and other disorders of sleep (pp. 56-91). Chicago, IL: W. T. Keener.
Mackenzie, S. (1887). Remarks on the value of Indian hemp in the treatment of a certain type of headache. The British medical Journal, 1(1359), 97-98.
Marihuana. (1950). In The Merck manual of diagnosis and therapy. A source of ready reference for the physician (8th ed., p. 1102). Rahway, NJ: Merck & Co.
Mathew, R. J., Wilson, W. H., Humphreys, D. F., Lowe, J. V., & Wiethe, K. E. (1992). Regional cerebral blood flow after marijuana smoking. Journal of Cerebral Blood Flow and Metabolism, 12(5), 750-758.
Mathew, R. J., Wilson, W. H., & Tant, S. R. (1989). Acute changes in cerebral blood flow associated with marijuana smoking. Acta Psychiatrica Scandinavica, 79(2), 118-128.
Mattison, J. B. (1973). Cannabis indica as an anodyne and hypnotic. In T. H. Mikuriya (Ed.), Marijuana: Medical papers 1839-1972 (pp. 151-157). Oakland, CA: Medi-Comp Press. (Reprinted from The St. Louis Medical and Surgical Journal, 56(5), pp. 256-271, by J. B. Mattison, 1891, November).
Mayor’s Committee on Marihuana. (1944). The marihuana problem in the city of New York: Sociological, medical, psychological and pharmacological studies. Lancaster, PA: The Jaques Cattell Press.
McGregor-Robertson, J. (1907). Indian hemp. In The household physician: A family guide to the preservation of health and the domestic treatment of illness (Vol. 4, p. 438). London: Gresham Publishing Company.
McMeens, R. R. (1973). Report of the Ohio State medical committee on canabis indica. In T. H. Mikuriya (Ed.), Marijuana: Medical papers 1839-1972 (pp. 117-140). Oakland, CA: Medi-Comp Press. (Reprinted from Transactions of the fifteenth annual meeting of the Ohio state medical society at Ohio White Sulphur Springs, June 12 to 14, 1860, pp. 75-100, by R. R. McMeens, 1860).
McPartland, J. M., & Russo, E. B. (2006). Cannabis and cannabis extracts: Greater than the sum of their parts? In E. B. Russo & F. Grotenhermen (Eds.), Handbook of cannabis therapeutics: From bench to bedside (pp. 171-204). Binghamton, NY: The Haworth Press Inc..
Melamede, R. (2005). Harm reduction – the cannabis paradox. Harm Reduction Journal, 2(17), 1-13. doi:10.1186/1477-7517-2-17
Mikuriya, T. H. (1969). Marijuana in medicine: Past, present, and future. California Medicine, 110, 34-40.
Mikuriya, T. H. (Ed.). (1973). Marijuana: Medical papers 1839-1972. Oakland, CA: Medi-Comp Press.
Mikuriya, T. H. (1998). Medicinal uses of cannabis. Retrieved November 25, 2011 from http://www.mikuriya.com/cw_meduses.html
Moore, T. H. N., Zammit, S., Lingford-Hughes, A., Barnes, T. R. E., Jories, P. B., Burke, M., et al. (2007). Cannabis use and risk of psychotic or affective mental health outcomes: A systematic review. Lancet, 370, 319-328.
Moreau, J. J. (1973). Hashish and mental illness (H. Peter & G. G. Nahas, Eds., G. J. Barnett, Trans.). New York: Raven Press. (Original work published 1845).
Müller, F. M. (Ed.). (1883). The Zend-Avesta: Part II: The Sîrôzahs, Yasts, and Nyâyis (J. Darmesteter, Trans.). In The sacred books of the East translated by various Oriental scholars (Vol. 23). Oxford: The Claredon Press.
Narcotic. (1990). In The Bantam medical dictionary (Rev. ed., pp. 285-286). New York: Bantam Books.
Nolin, P. C., Kenny, C., Banks, T., Maheu, S., & Rossiter, E. (2002). Cannabis: Our position for a Canadian public policy. Report of the Senate Special Committee on Illegal Drugs. Ottawa: Senate of Canada.
O’Neil, M. J. et al. (Eds.). (2001). Cannabis. In The Merck index. An encyclopedia of chemicals, drugs, and biologicals (13th ed., p. 292). Whitehouse Station, NJ: Merck & Co., Inc.
Osol, A., & Farrar, G. E. Jr. (Eds.). (1947). Cannabis. In The dispensatory of the United States of America (24th ed., pp. 1381-1383). Philadelphia: J. B. Lippincott Company.
Pharmaceutical Society of Great Britain. (1934). Cannabis. In The British pharmaceutical codex, 1934: An imperial dispensatory for the use of medical practitioners and pharmacists (p. 270). London: The Pharmaceutical Press.
Pierce, R. V. (1895). Narcotics: Indian hemp (Cannabis Indica). In The people’s common sense medical adviser in plain English: Or, medicine simplified (54th ed., pp. 343-344). Buffalo, NY: World’s Dispensary Medical Association.
Pierce, R. V. (1935). The people’s common sense medical advisor in plain English: Or, medicine simplified (100th ed.). Buffalo, NY: World’s Dispensary Medical Association.
Price, C., Hemmingsson, T., Lewis, G., Zammit, S., & Allebeck, P. (2009). Cannabis and suicide: Longitudinal study. British Journal of Psychiatry, 195, 492-497. doi:10.1192/bjp.bp.109.065227
ProCon.org. (2011, December 23). 16 Legal Medical Marijuana States and DC. MedicalMarijuana.ProCon.org. Retrieved January 28, 2012 from http://medicalmarijuana.procon.org/view.resource.php?resourceID=000881
Rätsch, C. (2001). Marijuana medicine: A world tour of the healing and visionary powers of cannabis (J. Baker, Trans.). Rochester, VT: Healing Arts Press. (Original work published 1998).
Reiss, A. J., & Roth, J. A. (Eds.). (1993). Alcohol, other psychoactive drugs, and violence. In Understanding and preventing violence volume 1 national research council (pp. 182-220). Washington, DC: National Academy Press.
Robinson, R. (1996). The great book of Hemp: The complete guide to the environmental, commercial, and medicinal uses of the world’s most extraordinary plant. Rochester, VT: Park Street Press.
Robinson, V. (1946, August-September). Concerning cannabis indica. Ciba Symposia, 8(5-6), 378-386, 404.
Roest, A. M., Marten, E. J., de Jonge, P., & Denollet, J. (2010). Anxiety and risk of incident coronary heart disease: A meta-analysis. Journal of the American College of Cardiology, 56(1), 38-46. doi:10.1016/j.jacc.2010.03.034
Rubin, V. (1976). Cross-cultural perspectives on therapeutic uses of cannabis. In S. Cohen & R. C. Stillman (Eds.), The therapeutic potential of marijuana (pp. 1-17). New York: Plenum Medical Book Company.
Russo, E. (2001). Cannabis: A breed apart. In Handbook of psychotropic herbs: A scientific analysis of herbal remedies for psychiatric conditions (pp. 220-232). New York: The Haworth Herbal Press.
Russo, E. B. (2007). History of cannabis and its preparation in saga, science, and sobriquet. Chemistry and Biodiversity, 4, 1614-1648.
Russo, E. B. (2011). Taming THC: Potential cannabis synergy and phytocannabinoid-terpenoid entourage effects. British Journal of Pharmacology, 163, 1344-1364. doi:10.1111/j.1476-5381.2011.01238.x
Russo, E., & Guy, G. W. (2006). A tale of two cannabinoids: The therapeutic rationale for combining tetrahydrocannabinol and cannabidiol. Medical Hypotheses, 66, 234-246. doi:10.1016/j.mehy.2005.08.026
Russo, E. B., Guy, G. W., & Robson, P. J. (2007). Cannabis, pain, and sleep: Lessons from therapeutic clinical trials of Sativex®, a cannabis-based medicine. Chemistry & Biodiversity, 4, 1729-1743.
Schifferes, J. J. (1963). Narcotics. In Schifferes’ family medical encyclopedia (p. 349). New York: Pocket Books, Inc.
Selye, H. (1973). The evolution of the stress concept. American Scientist, 61(6), 692-699.
Selye, H. (1976). Forty years of stress research: Principal remaining problems and misconceptions. Canadian Medical Association, 115, 53-56.
Selye, H. (1998). A syndrome produced by diverse nocuous agents. The Journal of Neuropsychiatry and Clinical Neurosciences, 10(2), 230-231. (Reprinted from Nature, 138, p. 32, by H. Selye, 1936, July 4).
Shafer, R. P. (1972). Marihuana – A signal of misunderstanding. The official report of the National Commission on Marihuana and Drug Abuse. New York, NY: Signet.
Shedler, J., & Block, J. (1990). Adolescent drug use and psychological health: A longitudinal inquiry. American Psychologist, 45(5), 612-630.
Shen, B-J., Avivi, Y. E., Todaro, J. F., Spiro, A. III., Laurenceau, J-P., Ward, K. D., et al. (2008). Anxiety characteristics independently and prospectively predict myocardial infarction in men. The unique contribution of anxiety among psychologic factors. Journal of the American College of Cardiology, 51(2), 113-119. doi:10.1016/j.jacc.2007.09.033
Solomon, C. (1935). Prescription writing and formulary: The art of prescribing. Philadelphia: J. B. Lippincott Company.
Solomon, C. (1952). Cannabis. In Pharmacology and therapeutics (6th ed., p. 189). Philadelphia: J. B. Lippincott Company.
Squire, P. W. (1899). Cannabis indica. Indian hemp. In Companion to the latest edition of the British pharmacopoeia (17th ed., p. 179-181). London: J. & A. Churchill.
Squire, P. W. (1908). Cannabis indica. Indian hemp. In Squire’s companion to the latest edition of the British pharmacopoeia (18th, ed., pp. 314-317). London: J. & A. Churchill.
Squire, P. W. (1916). Cannabis indica. Indian hemp. In Squire’s companion to the British pharmacopoeia (19th, ed., pp. 381-384). London: J. & A. Churchill.
Stecher, P. G., Finkel, M. J., & Siegmund, O. H. (Eds.). (1960). Cannabis. In The Merck index of chemical and drugs: An encyclopedia for chemists, pharmacists, physicians, and members of allied professions (7th ed., p. 204). Rahway, NJ: Merck & Co..
Stecher, P. G., Windholz, M, & Leahy, D. S. (Eds.). (1968). Cannabis. In The Merck index. An encyclopedia of chemicals and drugs (8th ed., p. 201). Rahway, NJ: Merck & Co., Inc.
Stillé, A., Maisch, J. M., Caspari, C., & Maisch, H. C. C. (1894). Cannabis indica. In The national dispensatory containing the natural history, chemistry, pharmacy, actions, and uses of medicines (5th ed., pp. 393-396). Philadelphia: Lea Brothers & Co..
Stress. (1990). In The Bantam medical dictionary (Rev. ed., pp. 414-415). New York: Bantam Books.
Sulak, D. (2011). Introduction to the endocannabinoid system. In P. Armentano, Emerging clinical applications for cannabis and cannabinoids: A review of the recent scientific literature (4th ed., pp. 10-14). Washington, DC: NORML Foundation.
Taber, C. W., & Associates. (1952). Narcotic. In Taber’s cyclopedic medical dictionary (5th ed., pp. N-2 – N-3). Philadelphia: F. A. Davis Company.
Taylor, B. (1855). Lands of the Saracen; or, pictures of Palestine, Asia Minor, Sicily, and Spain (1st ed.). New York: G. P. Putnam & Co.
Tournier, M., Sorbara, F., Gindre, C., Swendsen, J. D., & Verdoux, H. (2003). Cannabis use and anxiety in daily life: A naturalistic investigation in a non-clinical population [Abstract]. Psychiatry Research, 118(1), 1-8. doi:10.1016/S0165-1781(03)00052-0
Trousseau, A., & Pidoux, H. (1880). Treatise on therapeutics (9th ed., Vol. 2). (D. F. Lincoln, Trans.). New York: William Wood & Company.
U.K. Home Office. (1968). Cannabis: Report by the advisory committee on drug dependence. Home Office, Her Majesty’s Stationery Office.
Venes, D., et al. (Eds.). (2001a). Anxiolytic. In Taber’s cyclopedic medical dictionary (19th ed., p. 138). Philadelphia: F. A. Davis Company.
Venes, D., et al. (Eds.). (2001b). Marijuana. In Taber’s cyclopedic medical dictionary (19th ed., p. 1242). Philadelphia: F. A. Davis Company.
Wade, A., & Reynolds, J. E. F. (Eds.). (1977). Cannabis. In Martindale the extra pharmacopoeia incorporating Squire’s companion (27th ed., pp. 296-298). London: The Pharmaceutical Press.
Walton, R. P. (1973). Description of the hashish experience. In T. H. Mikuriya (Ed.), Marijuana: Medical papers 1839-1972 (pp. 83-114). Oakland, CA: Medi-Comp Press. (Reprinted from Marihuana: America’s new drug problem, pp. 86-114, by R. P. Walton, 1938).
Warner, R., Taylor, D., Wright, J., Sloat, A., Springett, G., Arnold, S., et al. (1994). Substance use among the mentally ill: Prevalence, reasons for use, and effects on illness. American Journal of Orthopsychiatry, 64, 30-39.
Windholz, M., Budavari, S., Blumetti, R. F., & Otterbein, E. S. (Eds.). (1983). Cannabis. In The Merck index: An encyclopedia of chemicals, drugs, and biologicals (10th ed., p. 1728). Rahway, NJ: Merck & Co., Inc..
Young, F. L. (1988, September 6). Opinion and recommended ruling, findings of fact, conclusions of law and decision of administrative law judge. In The matter of Marijuana rescheduling petition, Docket No. 86-22 (pp. 57-59). Administrative Law Court of the Drug Enforcement Administration.
Zuardi, A. W., Cosme, R. A., Graeff, F. G., & Guimaraes, F. S. (1993). Effects of ipsapirone and cannabidiol on human experimental anxiety. Journal of Psychopharmacology, 7, 82-88.
Zuardi, A. W., Crippa, J. A. S., Hallak, J. E. C., Moreira, F. A., & Guimaraes, F. S. (2006). Cannabidiol, a Cannabis sativa constituent, as an antipsychotic drug. Brazilian Journal of Medical and Biological Research, 39(4), 421-429.
Zuardi, A. W., & Guimaraes, F. S. (1997). Cannabidiol as an anxiolytic and antipsychotic. In M. L. Mathre (Ed.), Cannabis in medical practice: A legal, historical and pharmacological overview of the therapeutic use of marijuana (pp. 133-141). Jefferson, NC: McFarland.
Zuardi, A. W., Shirakawa, I., Finkelfarb, E., & Karniol, I. G. (1982). Action of cannabidiol on the anxiety and other effects produced by delta 9-THC in normal subjects. Psychopharmacology, 76, 245-250.
Images on pages 1, 6, and 26 from http://herbmuseum.ca/ taken by Bert Easterbrooke.
Image on page 5 from http://cannabishuman.bizland.com/cannabishumannakedtruth/id81.html
Image on page 8 from http://antiquecannabisbook.com/chap4/Mulford.htm
Image on page 9 from http://www.electricemperor.com/eecdrom/HTML/EMP/12/ECH42_03.HTM
Image on page 11 from http://antiquecannabisbook.com/chap5/HomeBrewB.htm
Images on pages 13, 17, 35, and 36 from Herb Museum taken by Bert Easterbrooke.
Images on pages 18-19 from http://antiquecannabisbook.com/chap7/CGrimault.htm
Image on page 22 from http://antiquecannabisbook.com/chap9/Migraine.htm
Postcards on pages 24 and 27 from Herb Museum, Vancouver, BC.
For more on the history of cannabis as a medicine,
information on its proper use to reduce potential harm, and evidence to disprove common myths, please refer to
For Membership and Access to Cannabis for Medical Purposes, Please Come and See Us at 1353 East 41st Avenue, Vancouver BC V5W 1R1 or visit us online at www.stressedanddepressed.ca.